2022 Post Graduate Convention

The 2022 Post Graduate Convention is supported in part by an educational grant from Alcon.
In Person Meeting in 2022!
Our 2022 event will be in person! This event will also be live streamed.
2022 Exhibitors
Thank you to our 2022 Exhibitors! Please visit them at the World Forestry Center in person or online if you are live streaming the conference.
Date & Location
Friday, March 11, 2022 | 8:00 AM to 5:00 PM (President’s Reception 5:00 PM)
Saturday, March 12, 2022 | 8:00 AM to 3:00 PM
World Forestry Center
4033 SW Canyon Rd
Portland, OR 97221
Proof of Vaccination Required
OAO is committed to your safety at the 2022 Post Graduate Convention. Therefore, our Board of Directors has determined that proof of COVID-19 vaccination will be required for everyone attending the meeting in person at the World Forestry Center
All 2022 attendees — OAO members and staff, our contractors, exhibitors and guests — will all be required to show proof of vaccination before being allowed to enter the conference area.
SAVE TIME – provide proof of vaccination when you complete your online registration. You may also email your vaccination card to staff@oregoneyephysicians.org.
Registration
Click here to register for the 2022 PGC.
Note: In order to take advantage of the significant member discounts on registration fees, OAO 2022 member dues must be paid prior to registration.
Materials
- 2022 Agenda
- 2022 PGC Program – high-res version | low-res version
- Online Course Evaluation
- PGC Course Checklist
Questions for Faculty
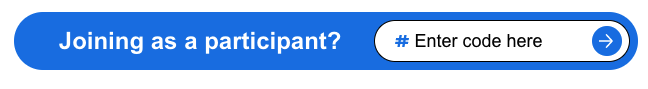
When the event starts, you can send in your questions for faculty, from the audience or at home, anonymously. Go to www.slido.com, enter #393447 and ask your question!
Live Stream Link
You will receive a link to the Live Stream via the email address you used to sign up for the Post Graduate Convention.
Parking Passes
Parking passes may be picked up at the PGC STOP sign on your way up to Cheatham Hall (PCC students will be standing outside) or from the OAO registration desk.
Target Audience
This activity has been planned for ophthalmology physicians (practicing and retired), and residents in the Pacific Northwest.
CME Certificate: In-Person
Step 1: Complete Online Course Evaluation
After the meeting, click on this link to complete your Online Course Evaluation. This evaluation can only be completed in one sitting (cannot do one course at a time). Please complete by midnight on Sunday, March 13th. If you need more time, please email Shelley at staff@oregoneyephysicians.org.
Step 2: CME Certificate will be Emailed
The OAO office will send you (via email) a certificate for you to complete and return. Please feel free to contact us if you have not yet received your certificate: staff@oregoneyephysicians.org.
CME Certificate: Live Stream
Step 1: Complete Online Course Evaluation
After the meeting, click on this link to complete your Online Course Evaluation. This evaluation can only be completed in one sitting (cannot do one course at a time). Please complete by midnight on Sunday, March 13th. If you need more time, please email Shelley at staff@oregoneyephysicians.org.
Step 2: Statement of Attendance
Send an email to OAO staff stating that you attended the Live Stream version of the OAO 2022 Post Graduate Convention, the number of hours you attended and the number of CME you will be claiming. Credit hours for each course are listed in the program and on the course checklist. Please complete by midnight on Sunday, March 13th. If you need more time, please email Shelley at staff@oregoneyephysicians.org.
Step 3: CME Certificate will be Emailed
The OAO office will send you (via email) a certificate for you to complete and return. Please feel free to contact us if you have not yet received your certificate: staff@oregoneyephysicians.org.
Accreditation
Accreditation Statement: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (AACME) through the joint providership of the Oregon Medical Association (OMA) and the Oregon Academy of Ophthalmology. The OMA is accredited by the AACME to provide continuing medical education for physicians.
AMA Credit Statement: The Oregon Medical Association designates this live activity for a maximum of 13.25 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
2022 Faculty & Lectures
Cornea | Mark J. Mannis, MD
University of California, Davis Eye Center
Professor and Chair, Department of Ophthalmology & Vision Science
Sacramento, CA
- Keratoplasty: Past, Present and Back to the Future
- Ophthalmology Through the Cornea: Lessons I Have Learned
- Rosacea: Common and Commonly Missed
- Case Study: Dendritic Dilemmas… and Other Cornea Mysteries
Disclosure: Mark J. Mannis, MD does not have any financial relationships with any ineligible companies.
Click here to see bio.
Glaucoma | Tosin Smith, MD
Clinician and Surgeon, Glaucoma Associates of Texas
Associate Professor, University of Texas Southwestern
Colleyville, TX
- Minimally Invasive Glaucoma Surgery: The Journey, Current Options and the Future
- A New Horizon in Glaucoma Medical Management: Sustained Release and Other Drug Delivery Platforms and De Novo Mechanisms of Action
- Office Tips and Tricks: Improving Clinical Workflow and Efficiency
- Case Study: A Day in the Life of a Glaucoma Surgeon: Cases from the Archives
Disclosures:
- Aerie | Consultant/Advisory Board, Speaker Bureau
- AGS | Research
- Alcon | Consultant/Advisory Board
- Allergen | Consultant/Advisory Board, Speaker Bureau, Research
- Bausch + Lomb | Consultant/Advisory Board, Speaker Bureau
- Glaukos | Consultant/Advisory Board, Research
- Iridex | Consultant/Advisory Board
- New World Medical | Consultant/Advisory Board
- Santen | Consultant/Advisory Board, Research
Click here to see bio.
Oculoplastics | Jeremiah Tao, MD
Gavin Herbert Eye Institute, University of California, Irvine
Professor and Chief, Division of Oculofacial Plastic and Orbital Surgery
Irvine, CA
- New Directions in Ocular Prosthetics
- When They Go Low: Management of Lower Eyelid Retraction
- Avoiding Disaster in Oculofacial Surgery
- Case Study: Oculoplastic Surgery Conundrums
Disclosure: Jeremiah Tao, MD does not have any financial relationships with any ineligible companies.
Click here to see bio.
Neuro-Ophthalmology | Michael S. Lee, MD
Professor, Departments of Ophthalmology, Neurology and Neurosurgery
Mackall-Scheie Endowed Chair
Program Director, Ophthalmology Residency Program
University of Minnesota
Woodbury, MN
- Evaluation and Management of Papilledema
- Approach to Patient with Eye Pain with a Normal Eye Exam
- Practical Assessment of Patient with Vision Loss and Normal Exam
- Case Study: Interactive and Interesting Neuro-Ophthalmology Cases
Disclosures:
- Horizon Therapeutics | Consultant/Advisory Board, Individual Stocks
- Pfizer | Individual Stocks
Click here to see bio.
Cultural Competency | Figure 8 Consulting
April D. Lewis, BA, MS & Carol D. French, BA, MA
Figure 8 Consulting, Portland, OR
- Culturally Responsive Health Care Delivery
Disclosure: April D. Lewis and Carol D. French do not have any financial relationships with any ineligible companies.
Click here to see bio.
Planning Committee/Staff Disclosures
- Planning Committee Disclosures:
- Andreas Lauer, MD
- Genentech | Research
- Biogen | Consultant, Research
- Steven Mansberger, MD
- Abbvie(Allergan) | Research
- Thea | Consultant
- Nicox | Consultant
- All other planners and contributors in a position to control content have no relationships with Ineligible Companies to disclose
- Andreas Lauer, MD
- All conflicts of interest have been mitigated and resolved
Course Descriptions & Objectives
Keratoplasty: Past, Present and Back to the Future | Mark J. Mannis, MD
This course will be a review of how current transplant procedures evolved.
- Understand how keratoplasty developed.
- Determine indications for each procedure.
- Have a better concept of future developments.
Ophthalmology Through the Cornea: Lessons I Have Learned | Mark J. Mannis, MD
Case presentations emphasizing the role of the cornea.
- Evaluate the role of the cornea in other specialties of eye care.
- Recognize less common clinical entities.
- Consider the key role of the cornea in non-corneal procedures.
Rosacea: Common and Commonly Missed | Mark J. Mannis, MD
Review of signs, symptoms and treatment of ocular rosacea.
- Recognize signs and symptoms of rosacea.
- Understand diagnostic criteria.
- Understand treatment paradigms.
Case Study: Dendritic Dilemmas… And Other Cornea Mysteries | Mark J. Mannis, MD
Case presentations illustrating different dendriform lesions.
- Distinguish lesions that present as dendrites.
- Develop appropriate management protocols.
- Recognize rare clinical presentations.
Minimally Invasive Glaucoma Surgery: The Journey, Current Options and the Future | Tosin Smith, MD
A review of currently available and future MIGS options, outcomes, associated adverse events and long term efficacy.
- Identify available and future MIGS procedures and outcomes.
- Recognize adverse events after MIGS procedures.
- Characterize the best MIGS practices including patient selection.
A New Horizon in Glaucoma Medical Management: Sustained Release and 0ther Drug Delivery Platforms and De Novo Mechanisms of Action | Tosin Smith, MD
Overview of newer glaucoma medications, sustained release and other delivery platforms as well as preservative free options.
- Identify new Glaucoma medications and their mechanism of action.
- Recognize available options of preservative free medications in medical management of glaucoma.
- Identify the currently pipeline for sustained release and drug delivery options for glaucoma medical management and their mechanism of action. Recognize adverse events after MIGS procedures.
Office Tips and Tricks: Improving Clinical Workflow and Efficiency | Tosin Smith, MD
A review of some office best practices that could optimize clinic flow and efficiency.
- Identify certain office practices that may interfere with office flow and efficiency.
- Recognize ways of addressing some of these issues in their practices.
Case Study: A Day in the Life of a Glaucoma Surgeon: Cases from the Archives | Tosin Smith, MD
A review presentation and clinical findings and treatment of a potpourri of clinical and surgical glaucoma cases.
- Recognize unusual presentation of certain types of complex glaucoma cases.
- Identify complications of medical and surgical glaucoma management
- Learn new surgical techniques for optimizing traditional glaucoma surgery
New Directions in Ocular Prosthetics | Jeremiah Tao, MD
Loss of an eye due to trauma or disease can lead to disfigurement. This course will explore methods and options in rehabilitating an anophthalmic socket so that prosthetic wearers feel less self-conscious about their appearance.
- Improve decision making about orbital volume implants.
- Incorporate surgical techniques that may improve prosthetic motility and implant retention outcomes.
- Understand the concept of a digital prosthetic eye.
When They Go Low: Management of Lower Eyelid Retraction | Jeremiah Tao, MD
Lower eyelid retraction has both esthetic and medical implications. Dry eye symptoms and blurred vision are frequent and the ocular surface may be at risk. The associated inferior scleral show and rounding of the lower eyelid may be disfiguring. This course will characterize the management of this common condition.
- Understand different vectors of lower eyelid retraction.
- Temporize ocular exposure when eyelid retraction develops acutely.
- Characterize various surgical interventions and their indications.
Avoiding Disaster in Oculofacial Surgery | Jeremiah Tao, MD
This course will explore several adverse in oculofacial surgery and how to avoid them.
- Understand how a surgical fire occurs and implement measures to prevent it.
- Be aware of the phenomenon of sneezing after propofol sedation and a needle near the eye and mitigate it risks.
- Understand which antiseptic surgical prep solutions to avoid in the periocular region.
- Implement measures to forestall an iatrogenic central retinal artery occlusion.
Case Study: Oculoplastic Surgery Conundrums | Jeremiah Tao, MD
This course will review patients with difficult oculofacial conditions or injuries.
- Understand limitations in treatment of filler induced blindness.
- Prevent lagophthalmos after blepharoplasty.
- Manage filler and other foreign material granulomas.
Evaluation and Management of Papilledema | Michael S. Lee, MD
This lecture will review best practices for distinguishing pseudopapilledema and papilledema. The current diagnostic criteria for pseudotumor cerebri will be discussed. Finally, the lecture will conclude with discussion of the medical and surgical management of pseudotumor cerebri.
- Determine testing strategies for differentiating pseudopapilledema and papilledema.
- Describe the diagnostic criteria for pseudotumor cerebri.
- Know the indications for surgical intervention among patients with pseudotumor cerebri.
Approach to the Patient with Eye Pain with a Normal Eye Exam | Michael S. Lee, MD
This lecture will review a focused history and examination of the patient with eye pain. It will then identify when and how to order neuroimaging followed by a case-based approach to various causes of eye pain including photophobia, post-LASIK pain, painful Horner syndrome, and various forms of neuralgia, among others.
- Recognize how to diagnose and treat trochleitis.
- Understand that dry eye syndrome is the most common cause of eye pain.
- Identify indomethacin as the treatment of choice for hemicrania continua.
Practical Assessment of the Patient with Vision Loss and Normal Exam | Michael S. Lee, MD
This lecture will review the use of visual fields in the evaluation of unexplained vision loss. It will also discuss techniques to assess nonorganic vision loss. Finally, a review of how to use ancillary testing to evaluate the visual system including when to obtain neuroimaging will be performed.
- Describe the use of visual fields as a first step in the diagnostic approach to unexplained vision loss.
- Understand when the diagnosis of nonorganic vision loss is appropriate.
- Differentiate between an optic neuropathy and retinopathy.
Case Study: Interactive and Interesting Neuro-Ophthalmology Cases | Michael S. Lee, MD
This is a case-based discussion between the learners and the lecturer. Cases will focus on how to think about the approach and not just the final diagnosis.
- Discuss the approach to the patient with vision loss and optic disc edema.
- Understand how to manage intractable diplopia.
- Describe the diagnosis and management of downbeat nystagmus.
Culturally Responsive Health Care Delivery | April Lewis, BA, MS & Carol French, BA, MA
Use the cultural agility model (self-awareness, curiosity and empathy) to understand how cultural agility improves the delivery of culturally responsive care and to identify and describe how cultural factors and unconscious bias impact clinical interactions and outcomes.
- Identify and describe how cultural factors and unconscious bias impact clinical interactions and outcomes.
- Describe ways to build and sustain non-judgmental and respectful clinical interactions and environments.
- Understand that health care should be designed to meet the needs of ALL of society’s members and that clinical encounters must accommodate patient autonomy and must not devalue nor marginalize minorities.
Cancellations
Cancellation requests must be submitted in writing. There is a $50.00 fee for cancellation before Feb 25th, 2022. There are no refunds for cancellations after Feb 25th, 2022.




